
Building Analytics-Ready Data Infrastructure for Hospital CIOs
Mownika
15th OCt 2025
Talk to our cloud experts
Subject tags
The increasing complexity of healthcare data presents a significant challenge for hospital Chief Information Officers (CIOs), who must strike a delicate balance between operational efficiency and improving patient care.
This blog explores the pivotal role CIOs play in developing and managing the data infrastructure that is essential for informed decision-making, streamlined workflows, and improved patient care.
Key Takeaways
- Hospital CIOs play a crucial role in building and managing data infrastructure, ensuring seamless integration, and utilizing data for informed decision-making.
- Healthcare data is often fragmented, with clinical, operational, and patient-generated data originating from disparate sources, which poses significant integration challenges.
- Key components of an analytics-ready infrastructure include scalable storage, seamless EHR integration, robust data governance, and strong security protocols.
- Cloud computing, AI, and machine learning are pivotal technologies accelerating healthcare data infrastructure, enhancing efficiency, and improving patient outcomes.
- Data quality standards and continuous monitoring are crucial for ensuring reliable insights and driving effective healthcare analytics.
Understanding the Current Data Landscape in Healthcare
Healthcare data is generated from a wide array of sources, creating vast silos of information that can limit the ability to integrate systems and extract meaningful insights. This fragmentation of data represents a significant barrier for healthcare organizations looking to become truly data-driven.
Hospitals generate several types of data, each serving different functions:
- Clinical Data: This includes electronic health records (EHRs), medical imaging, laboratory results, and prescriptions.
- Operational Data: Covers resource utilization, staffing, and financial data, all critical for hospital management.
- Patient-Reported Data: Comes from patient portals, surveys, and mobile health apps.
Despite the growing reliance on these diverse data streams, healthcare systems face significant challenges in accessing and integrating data, such as:
- Data Fragmentation: EHRs often lack integration with other hospital systems (e.g., lab results, pharmacy data, financial tools).
- Patient-Generated Data: Data from wearables and health apps often resides in separate systems, making it difficult to get a comprehensive view of the patient.
- Unstructured Data: Clinical notes and imaging data are often unstructured and hard to process into actionable insights.
With a clear understanding of the landscape, let's examine the essential components needed to establish an analytics-ready data infrastructure for hospitals.
Key Components of Analytics-Ready Data Infrastructure

Building an analytics-ready data infrastructure is crucial for healthcare organizations seeking to improve patient outcomes and optimize operational efficiency.
To achieve this, CIOs must focus on key elements such as data storage, integration, governance, and security to ensure smooth interoperability and regulatory compliance.
Data Warehousing and Storage Solutions
Hospitals require scalable, flexible data storage solutions that can accommodate a diverse range of data types, including structured, semi-structured, and unstructured data.
Solutions such as hybrid cloud models offer flexibility and scalability, combining cloud storage with on-premises systems.
These solutions support a variety of data types, ensuring that hospitals can manage large volumes of data without compromising security or accessibility.
Integration with Electronic Health Records (EHR)
Seamless integration with EHRs is essential for creating a unified patient view. Standards like FHIR (Fast Healthcare Interoperability Resources) and HL7 are fundamental in ensuring that data can flow between disparate healthcare systems in a structured and meaningful way.
- Real-time data ingestion from EHRs is vital to provide clinicians with the most up-to-date information during patient encounters.
Data Governance and Compliance Requirements
Hospitals must adhere to HIPAA, HITECH, and other compliance regulations. Establishing data governance frameworks ensures that data is accurate, consistent, and securely managed.
- Implementing automated compliance monitoring and data lineage tracking is crucial for maintaining transparency and accountability in healthcare systems.
Security and Privacy Considerations in Healthcare Data
Securing patient data is essential not only for regulatory compliance but also for building trust with patients and safeguarding sensitive health information.
Hospitals must implement:
- Encryption to secure data both at rest and in transit.
- Access Controls to restrict data access to authorized personnel.
- Zero Trust Security Models to enforce strict security protocols across all systems.
Now, let’s examine the tools and technologies that can help accelerate the implementation of healthcare data infrastructure.
How to Accelerate Healthcare Data Infrastructure with Modern Technologies
Building a robust data infrastructure in healthcare requires adopting tools that streamline data integration, processing, and analysis. Cloud computing, machine learning, and data management platforms are essential in transforming raw healthcare data into actionable insights.
These technologies enable hospitals to boost efficiency, enhance decision-making, and improve patient care outcomes.
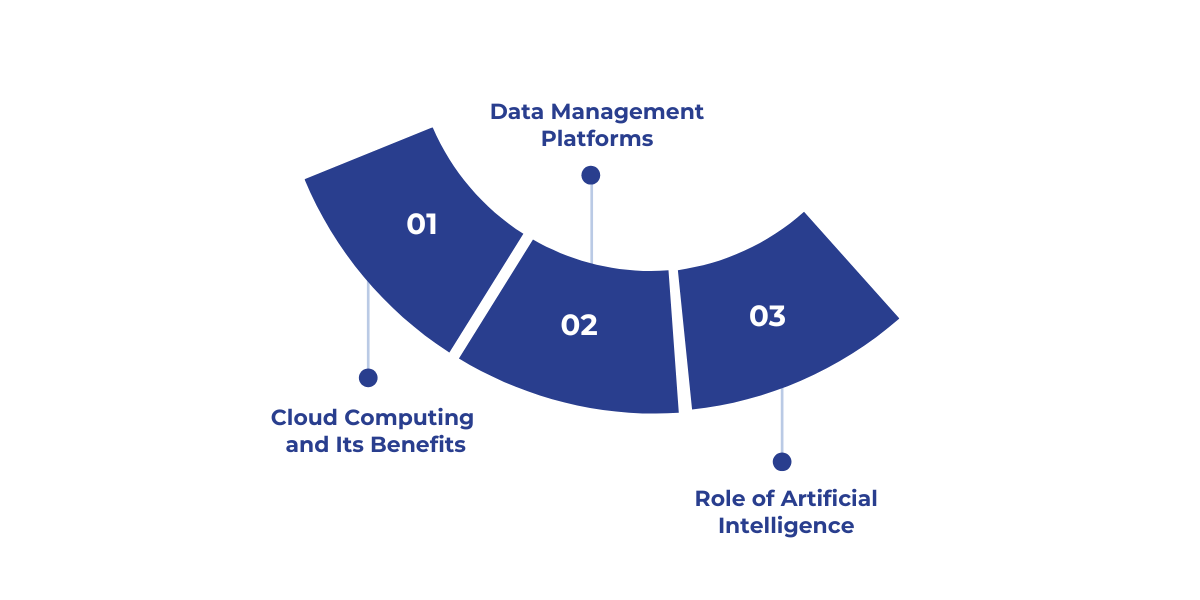
1. Cloud Computing and Its Benefits
Cloud computing enables hospitals to scale their data storage and processing capabilities quickly and cost-effectively, eliminating the need for significant capital investment in on-premises infrastructure.
Leading cloud platforms, such as Microsoft Azure, provide healthcare-specific solutions that meet stringent industry standards, including HIPAA and HITECH, ensuring compliance and security.
2. Data Management Platforms
Data management platforms, such as Arcadia, Health Catalyst, and IBM Watson Health, play a crucial role in enabling hospitals to manage and integrate large, disparate datasets.
These platforms support predictive analytics and clinical decision support, enabling healthcare organizations to extract actionable insights from complex data and enhance patient care while optimizing hospital operations.
3. Role of Artificial Intelligence and Machine Learning in Data Processing
Artificial intelligence (AI) and machine learning (ML) technologies are increasingly being used to automate tasks such as data cleaning, identify hidden patterns, and enhance diagnostic accuracy.
AI and ML tools can predict patient outcomes, optimize resource allocation, and personalize care, significantly contributing to improved hospital operations and more effective treatment plans for patients.
To put this into action, it's important to follow a structured approach when implementing a robust data infrastructure across your organization.
Steps for Implementing an Effective Data Infrastructure
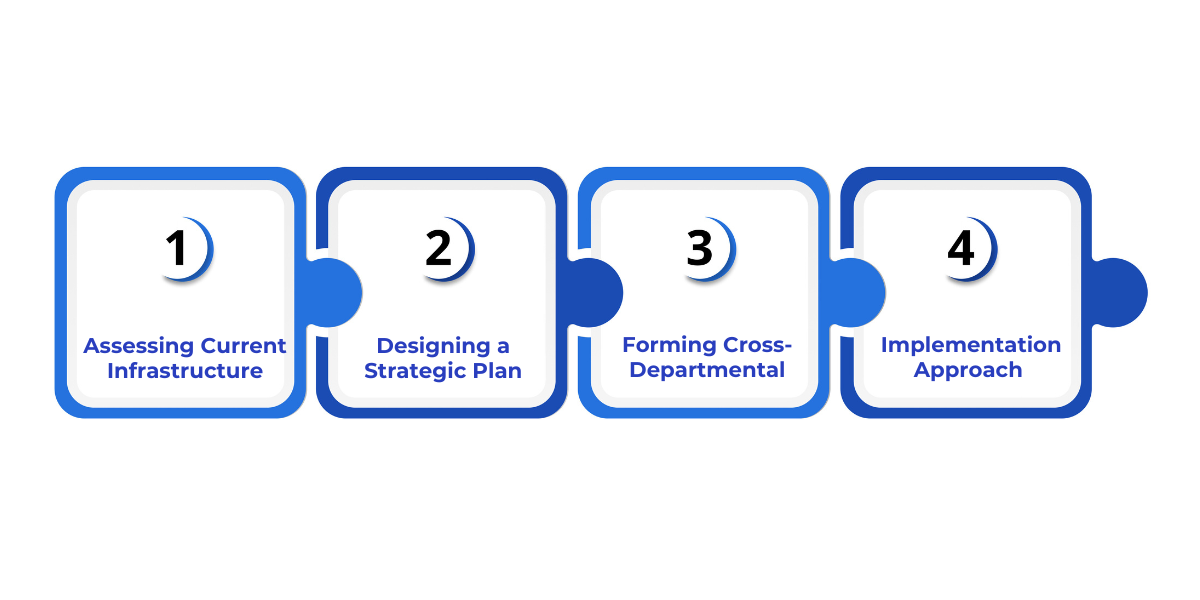
Building an analytics-ready data infrastructure is a multi-step process. CIOs must begin by assessing their current systems, identifying gaps, and then implementing an actionable roadmap to address these gaps.
The process should be approached in phases to ensure gradual, manageable improvements.
1. Assessing Current Infrastructure and Identifying Gaps
Begin by conducting a thorough audit of existing systems and infrastructure. Identify where there is a lack of integration, inefficiencies in data handling, or security vulnerabilities.
2. Designing a Strategic Plan for Infrastructure Development
Develop a strategic plan with clear, well-defined short-term and long-term objectives. Focus on improving interoperability, ensuring compliance, and optimizing data storage.
3. Forming Cross-Departmental Teams for Implementation
Data infrastructure projects require collaboration between clinical teams, IT, and administrative units. Cross-departmental teams ensure that the infrastructure meets all hospital requirements and that all stakeholders are aligned on goals.
4. Phased Implementation Approach: Short-term and Long-term Goals
Start with high-impact, low-complexity projects that show quick wins. Gradually expand the scope of the project, integrating more complex data sources and technologies as the system matures.
As you implement infrastructure, maintaining high-quality data is crucial. Here’s how to ensure data quality remains consistent and actionable.
Ensuring and Maintaining High-Quality Data for Effective Healthcare Analytics
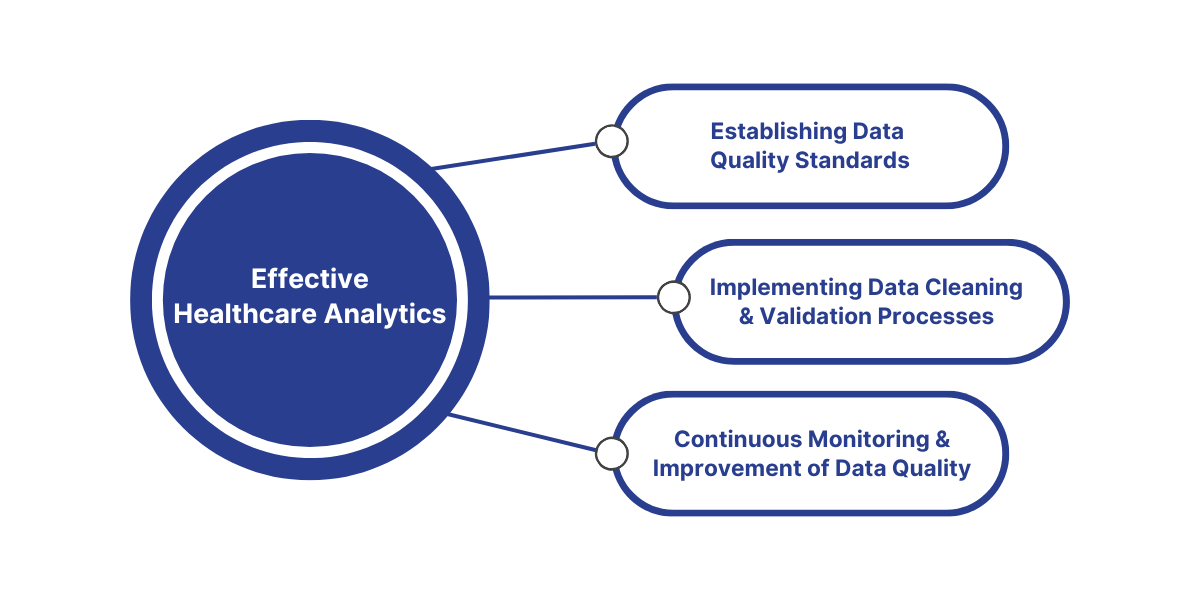
The effectiveness of healthcare data analytics relies heavily on the quality of the data itself. To ensure that data systems remain reliable and actionable, it's crucial to establish data quality standards and implement continuous monitoring.
This helps maintain the integrity of clinical, operational, and patient-reported data, ensuring that insights drawn from it are accurate and reliable.
1. Establishing Data Quality Standards
Define and enforce clear standards for data accuracy, consistency, and completeness across all systems to ensure reliable data. These standards should cover clinical, operational, and patient-reported data to ensure uniformity and reliability.
2. Implementing Data Cleaning and Validation Processes
Utilize automated tools to clean and validate incoming data. These tools help identify discrepancies in real-time, resolving inconsistencies and ensuring that data remains accurate and actionable.
3. Continuous Monitoring and Improvement of Data Quality
Data quality should be constantly monitored, with ongoing improvements based on regular feedback from stakeholders. Establish key performance indicators (KPIs) to track data quality and ensure it consistently meets the set standards.
After establishing the infrastructure, it’s vital to understand how healthcare data analytics directly impacts patient outcomes and operational efficiency.
How Healthcare Data Analytics Impacts Outcomes
Healthcare data analytics plays a pivotal role in improving patient outcomes and operational efficiency. By analyzing vast amounts of healthcare data, organizations can uncover patterns, predict trends, and make informed decisions that lead to better care delivery and healthier patients.
Personalized Care
By analyzing individual patient data, healthcare providers can tailor treatments to meet the specific needs of each patient.
This personalized approach increases the chances of successful outcomes, as treatments are tailored to individual factors such as medical history, lifestyle, and treatment response.
Predictive Healthcare
Analytics can identify patterns in historical data to predict future health events, such as disease outbreaks or patient deterioration.
This predictive power enables healthcare systems to take proactive measures, reducing complications, lowering healthcare costs, and saving lives.
Operational Efficiency
Data analytics optimizes hospital operations by streamlining workflows and improving resource allocation.
Predictive models can forecast patient volume, helping hospitals adjust staffing levels and manage resources more efficiently. This results in faster care and better overall hospital performance.
Quality of Care
Continuous monitoring and benchmarking against industry standards help improve the quality of care.
By tracking patient outcomes and measuring the effectiveness of treatments, healthcare organizations can pinpoint areas for improvement and ensure ongoing enhancement of care delivery.
Effective implementation and integration of data systems requires strong leadership. Let’s look at how Hospital CIOs manage the change process.
The Important Role of Hospital CIOs in Managing Change
Hospital Chief Information Officers (CIOs) play a crucial role in successfully implementing analytics-ready data infrastructures.
They not only oversee the technological transition but also manage cultural shifts, ensuring that the organization adopts a data-driven approach to decision-making while overcoming both technological and cultural barriers.
Conclusion
Advancements in integration and technology will drive the future of healthcare data analytics. Hospitals that invest in scalable, analytics-ready infrastructures will improve patient outcomes, optimize operations, and reduce costs.
With the rise of FHIR standards and edge computing, systems will be able to exchange data more effectively, enabling real-time diagnostics. AI-powered analytics and cloud-first strategies will further streamline operations and enhance care.
To implement a strong data infrastructure that delivers measurable results, WaferWire can guide your organization through the implementation of real-time data management, predictive analytics, and cloud solutions that directly improve patient care and hospital efficiency.
Contact us for a detailed consultation on how we can help your healthcare system achieve the power of data analytics.
FAQs
Q: What are the primary challenges hospitals face when integrating healthcare data?
A: The main challenges include data fragmentation, with clinical, operational, and patient-generated data often housed in separate systems. Additionally, unstructured data, such as clinical notes or imaging, is difficult to process, limiting actionable insights. Ensuring interoperability across various platforms remains a significant hurdle.
Q: How can CIOs ensure hospital staff adapts to the data-driven culture?
A: CIOs can promote data literacy by offering targeted training programs, ensuring that both clinical and administrative staff understand how to utilize data analytics tools. This includes making tools accessible and demonstrating their value in improving patient care and hospital operations.
Q: What role does artificial intelligence (AI) play in healthcare data infrastructure?
A: AI helps automate processes such as data cleaning, identifying patterns, and predicting patient outcomes. By leveraging machine learning, hospitals can optimize resource allocation, personalize care, and enhance diagnostic accuracy, ultimately improving operational efficiency.
Q: How can hospitals maintain data security while integrating new technologies?
A: Hospitals must implement robust encryption for data at rest and in transit, enforce access controls, and adopt a zero-trust security model. These steps ensure that patient data remains secure even as technologies like AI and cloud computing are integrated into hospital systems.
Q: What’s the role of cloud computing in modernizing healthcare data infrastructure?
A: Cloud computing allows hospitals to scale their data storage and processing capabilities quickly without heavy capital investment in on-premises infrastructure. Leading platforms offer healthcare-specific solutions, ensuring compliance with HIPAA and improving overall data accessibility and security.
Subscribe to Our Newsletter
Get instant updates in your email without missing any news

Copyright © 2025 WaferWire Cloud Technologies




.png)













