Healthcare Modernization Strategies: Key Benefits for the Future
Murthy
8th Oct 2025
Talk to our cloud experts
Subject tags
As healthcare systems face growing demands, outdated technology often leads to inefficiencies and delays in patient care. Legacy infrastructures, including non-interoperable Electronic Health Records (EHR), struggle to keep up with modern advancements.
Technologies like digital pathology and augmented reality (AR) surgery assistance are pushing the boundaries of precision in patient care.
This blog explores the challenges of legacy healthcare systems and strategies for modernization to enhance efficiency and care delivery.
Key Takeaways:
- Legacy healthcare systems create inefficiencies, security risks, and fragmented data, hindering care delivery.
- Modernizing with AI, cloud, and predictive analytics improves operational efficiency and enhances patient outcomes.
- Integration of tools like telemedicine, EHRs, and cloud-based solutions streamlines processes and ensures better care coordination.
- Modern systems reduce costs, improve regulatory compliance, and support personalized treatments.
- Future-proofing healthcare through modular systems, AI, and blockchain ensures adaptability to emerging technologies.
Why Healthcare Software Modernization is Necessary?

Legacy systems often lead to operational delays, fragmented data, and security vulnerabilities, hindering organizations' ability to meet modern healthcare demands. Upgrading these systems allows healthcare providers to streamline processes, enhance decision-making, and improve data security.
1. Manual Processes: Legacy systems rely on outdated manual tasks like data entry and billing, causing delays and errors. Modern systems automate these processes, improving accuracy and freeing up resources.
- Example: AI-driven scheduling optimizes appointment times, reducing downtime and improving resource use.
2. Fragmented Data vs. Integrated Solutions: Legacy systems often store patient data in isolated silos, making it difficult for healthcare providers to access comprehensive patient histories or real-time diagnostic information.
Modern software integrates various data streams (EHR, lab results, wearables) into a centralized platform, making vital information accessible to clinicians at the point of care.
3. Predictive Insights: Modern systems employ predictive analytics to identify potential health risks before they escalate. Machine learning algorithms analyze patient data trends, enabling proactive interventions that reduce the need for reactive care.
- Example: AI tools can analyze blood glucose patterns in diabetic patients and predict the likelihood of complications like diabetic retinopathy, allowing for earlier interventions.
Key Benefits of Healthcare Software Modernization

Modern healthcare software provides tangible benefits across the operational, financial, and clinical spectrums. These improvements directly impact patient outcomes, hospital revenue, and regulatory adherence.
1. Improved patient care
Modern healthcare systems are designed to enhance patient care by utilizing advanced technologies, such as AI, predictive analytics, and genomics, to offer timely interventions and personalized treatment plans.
-Clinical decision support systems (CDSS)
Modern systems integrate real-time clinical decision support tools that can alert healthcare providers to potential complications based on patient data.
For example, AI-based CDSS can notify clinicians about possible adverse drug interactions before prescriptions are finalized.
-Personalized medicine
Data analytics and genomics are transforming how treatments are tailored to individuals. Modern systems enable healthcare providers to store genomic data and use AI-driven tools to recommend the most effective treatments.
2. Cost savings
Healthcare organizations can significantly reduce operational expenses through automation, predictive analytics, and better resource utilization, leading to increased profitability and sustainability.
-Operational efficiencies
By automating tasks such as patient intake, claims processing, and resource allocation, healthcare organizations can significantly reduce labor costs and improve revenue cycle management.
-Optimizing resource usage
With predictive analytics, hospitals can better manage bed availability, staff scheduling, and equipment utilization, ensuring that they don’t over-invest in underutilized assets.
3. Regulatory compliance
Modern healthcare systems support strict adherence to regulatory standards by providing automated audit trails and real-time reporting capabilities, which streamline compliance processes.
-Automated audit trails
Modern healthcare systems generate real-time, immutable audit trails that track who accessed patient data, when, and for what purpose. This helps meet compliance requirements without manual intervention.
-Real-time reporting
With cloud systems, healthcare organizations can generate real-time compliance reports, ensuring that they are always ready for inspections or audits.
4. FHIR (Fast Healthcare Interoperability Resources)
Modern healthcare systems are designed to support open standards, such as FHIR, allowing for seamless data exchange across disparate systems.
This standard facilitates interoperability between different healthcare software, such as EHRs, lab systems, and imaging tools, improving care coordination.
As healthcare organizations embark on this transformation, the right features in modern software will determine the ultimate success of the initiative.
Key Features of Modern Healthcare Software
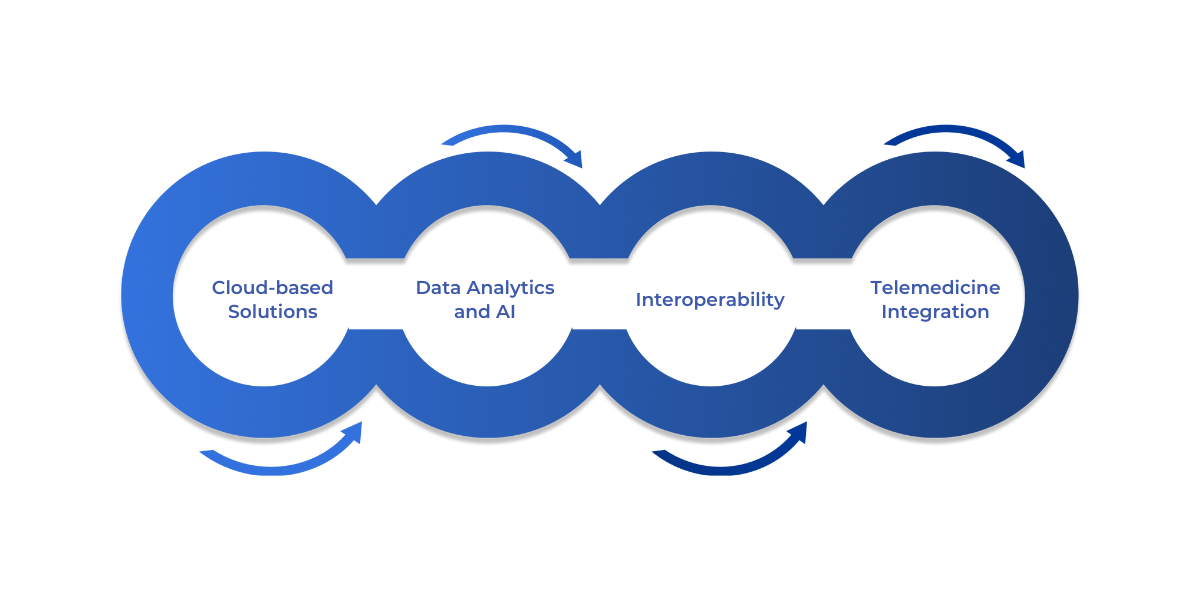
These technologies enable seamless collaboration, real-time data access, and predictive insights, ultimately leading to improved patient outcomes.
1. Cloud-based Solutions
Cloud-based platforms offer scalability and flexibility, enabling healthcare organizations to adjust their infrastructure to meet changing demands while ensuring high availability and disaster recovery.
- Scalability and flexibility: Cloud-based platforms enable healthcare organizations to scale their operations up or down based on demand, avoiding the costs and risks associated with on-premise infrastructure. Cloud computing providers also offer disaster recovery and high availability configurations, reducing downtime in critical healthcare systems.
- Collaborative capabilities: Cloud systems allow for collaborative care models where multiple specialists can work on the same patient case regardless of location, using shared access to up-to-date information.
2. Data Analytics and AI
Data analytics and AI tools are transforming healthcare software by enabling predictive insights, personalized care, and efficient decision-making.
- Predictive analytics: AI and machine learning tools in healthcare software can identify patterns in patient data to predict risks such as hospital readmissions or disease outbreaks. For example, AI tools can analyze imaging data to help detect early signs of cancer or neurological conditions.
- Natural language processing (NLP): NLP is used to extract actionable insights from unstructured data, such as clinical notes or patient feedback, further supporting diagnostic decisions and treatment plans.
3. Interoperability
Modern healthcare systems are designed to work seamlessly with various tools and platforms, ensuring the free flow of data across institutions and enhancing care coordination.
- HL7 and FHIR integration: Modern systems integrate seamlessly with other healthcare tools and platforms through HL7 (Health Level 7) and FHIR standards. This ensures that patient data can be shared across different institutions and providers without compatibility issues, thus enhancing continuity of care.
4. Mobile and Telemedicine Integration
Mobile and telemedicine integration enhances patient engagement by providing easy access to healthcare services and improving overall treatment adherence.
- Patient engagement: Mobile apps enable patients to access their medical records, schedule appointments, receive telemedicine consultations, and receive reminders for medication or upcoming checkups.
When considering the next steps in modernization, understanding the necessary strategies is key to ensuring smooth transitions and maximum benefits.
Strategies for Healthcare Software Modernization
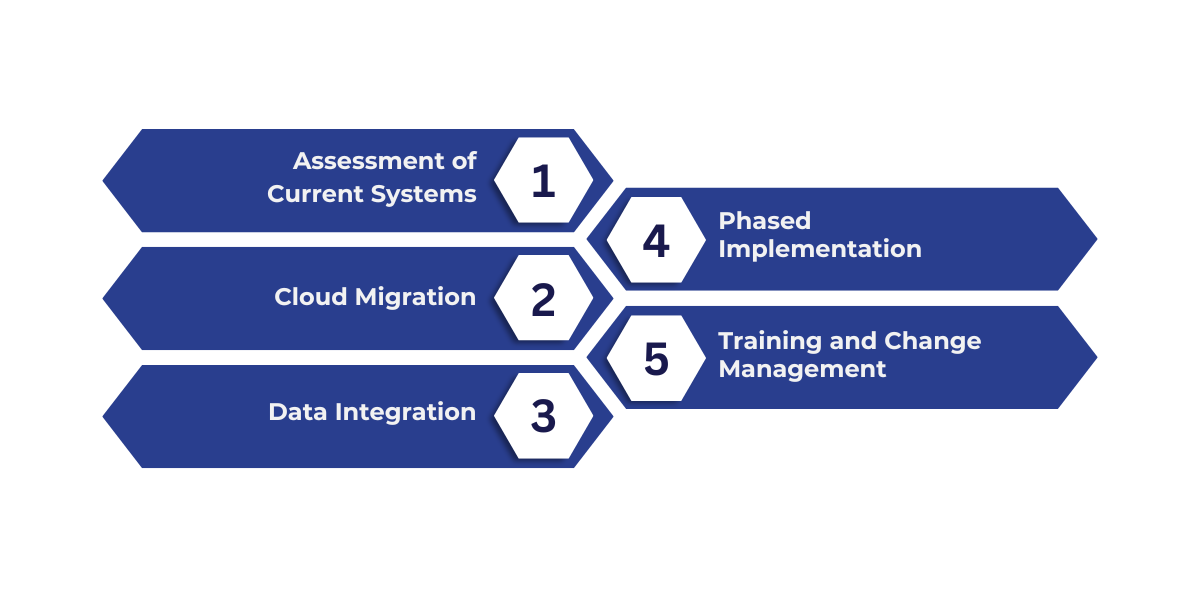
Successfully modernizing healthcare software requires a methodical approach, addressing key areas such as system assessment, cloud migration, data integration, and training. A structured strategy ensures minimal disruption while maximizing long-term benefits.
1. Assessment of Current Systems
Before initiating modernization, organizations must identify the deficiencies in existing systems. This includes evaluating performance, security risks, and interoperability challenges. The gap analysis informs decision-making for selecting suitable technologies and strategies.
Key Focus Areas:
- Performance: Evaluate system speed, scalability, and data processing capacity.
- Security: Assess vulnerabilities to ensure compliance with evolving regulations (e.g., HIPAA, GDPR).
- Interoperability: Identify limitations in connecting with other systems or sharing data across platforms.
Example: Conducting a gap analysis might reveal that an organization’s EHR system is not capable of integrating with external laboratory systems, causing delays in diagnostic information.
2. Cloud Migration
Migrating legacy systems to cloud-native platforms is a cornerstone of modernization. Cloud services offer scalability, enhanced security, and cost-efficiency compared to traditional on-premise infrastructure.
Key Benefits:
- Scalability: Adjust resource allocation dynamically to meet changing healthcare demands.
- Regulatory Compliance: Cloud providers, like AWS Healthcare, offer built-in tools and configurations that help organizations meet compliance standards such as HIPAA.
- Security: Advanced security features, including data encryption and multi-factor authentication, ensure patient data is protected in transit and at rest.
Example: Migrating to a cloud-based EHR system allows for easy integration with telemedicine platforms, providing seamless access to patient data during virtual consultations.
3. Data Integration
Modern healthcare systems require centralized data repositories to handle vast amounts of structured and unstructured data. Implementing data lakes enables the aggregation of diverse data types, such as EHRs, imaging data, and patient-generated data.
APIs (Application Programming Interfaces) are then used to connect these data lakes with external systems, ensuring smooth data exchange and accessibility across platforms.
Key Considerations:
- Data Quality: Ensure the integrity and accuracy of data before storing it in data lakes.
- Interoperability: Use standardized APIs, like HL7 and FHIR, to facilitate data exchange between systems.
- Real-Time Access: Enable real-time data sharing for clinical decision-making and patient care continuity.
Example: Integrating real-time data from wearable devices with EHRs using APIs allows clinicians to monitor patient health remotely and make timely interventions.
Also Read: Data Lakehouse Vs. Data Warehouse: Key Differences
4. Phased Implementation
Phased rollouts reduce the risk of system failures and allow for smoother transitions. Healthcare organizations should start with a small-scale implementation of new technologies, gathering feedback and making adjustments before full-scale deployment.
Key Steps:
- Pilot Testing: Deploy new systems in one department or unit to test functionality and identify challenges.
- Iterative Feedback: Collect feedback from users to address issues early on and fine-tune the system for broader implementation.
- Risk Mitigation: Minimizing the scope of initial deployment limits disruption to critical healthcare services.
Example: A healthcare organization could begin by implementing a new EHR system in the outpatient department and gradually expand it to inpatient services after addressing early-stage challenges.
5. Training and Change Management
Effective training programs are essential to ensure that healthcare staff can efficiently use the new systems. Ongoing support and feedback mechanisms help address concerns and ensure long-term success.
Key Elements:
- Role-Specific Training: Tailor training programs to specific roles, such as physicians, nurses, or administrative staff.
- 24/7 Support: Ensure that technical support is available at all times to address system issues or user queries.
- Feedback Loops: Establish channels for users to report issues and suggest improvements, fostering continuous system refinement.
Example: Organizing a series of workshops for physicians and nurses on how to use the new EHR system effectively, followed by a dedicated helpline for ongoing assistance.
Overcoming Challenges in Modernization
Healthcare software modernization presents several challenges, such as budget constraints, staff resistance, and data migration issues. Addressing these hurdles requires targeted strategies and the use of innovative tools.
The table below summarizes key challenges and corresponding solutions for overcoming them.
Future-proofing Healthcare IT Systems

To ensure longevity and adaptability, healthcare IT systems must be designed to integrate with emerging technologies like AI, blockchain, and the Internet of Medical Things (IoMT). The following strategies enable healthcare systems to remain flexible and ready for future innovations.
1. Modular Systems
Modular systems enable healthcare organizations to integrate new technologies without requiring a complete overhaul of their existing infrastructure.
For example, an AI-powered diagnostic tool can be seamlessly integrated into an existing Electronic Health Record (EHR) system, enhancing capabilities without disrupting other operations.
2. Scalable Infrastructures
Cloud-native infrastructures enable on-demand scaling, allowing healthcare organizations to grow without the need for significant upfront investments in physical infrastructure.
3. Integration with Emerging Technologies
Blockchain technology enhances data security by creating immutable records of patient data exchanges, ensuring that sensitive patient information is protected across decentralized networks.
Conclusion
By embracing modular systems, scalable infrastructures, and emerging technologies like AI, blockchain, and IoMT, healthcare providers can streamline operations, improve patient care, and ensure data security.
These advancements empower healthcare systems to not only meet current demands but also stay prepared for future challenges and innovations.
At WaferWire Cloud Technologies, we specialize in guiding organizations through this transformation, offering tailored cloud solutions and AI strategies to modernize healthcare IT systems efficiently.
Contact us today to discover how we can help future-proof your healthcare infrastructure and improve patient care delivery.
FAQs:
Q: How do healthcare organizations overcome staff resistance to new technology during modernization?
A: Overcoming resistance involves involving key stakeholders early, providing hands-on training, and ensuring ongoing support. Change management strategies, including clear communication and addressing concerns, are crucial to successful adoption.
Q: What challenges do healthcare providers face in migrating from legacy systems to the cloud?
A: The main challenges include data security concerns, integration complexities, and the need for comprehensive staff training. Successful migration requires careful planning, using tools to automate data transfer, and ensuring compliance with regulations.
Q: How does AI improve the accuracy of diagnoses in healthcare modernization?
A: AI-driven diagnostic tools analyze vast amounts of patient data, such as imaging and lab results, to detect early signs of diseases with higher accuracy. This reduces diagnostic errors, improves decision-making, and enables earlier intervention.
Q: What role does blockchain play in the future of healthcare systems?
A: Blockchain enhances data security by creating immutable records of patient information. It ensures secure, transparent data exchanges across decentralized systems, protecting sensitive patient data from breaches and unauthorized access.
Q: How can healthcare organizations ensure data integrity when integrating new technologies?
A: Ensuring data integrity involves using standardized APIs, conducting regular data audits, and implementing automated tools for seamless migration. Data quality and real-time access are prioritized to maintain accuracy and consistency during integration.
Subscribe to Our Newsletter
Get instant updates in your email without missing any news

Copyright © 2025 WaferWire Cloud Technologies




.png)