Improving Patient Risk Stratification with Modern Data Estates
Harish
15th Oct 2025

Talk to our cloud experts
Subject tags
Every day, hospitals generate huge amounts of data, from patient records and lab results to medical images and operational logs. Much of this data is stored in separate systems, making patient risk stratification slower and less accurate.
Microsoft Fabric helps hospitals consolidate all their data in one place, making it easier to analyze and take action. By combining different data sources and using real-time analytics, hospitals can improve patient risk stratification, spot high-risk patients faster, manage resources efficiently, and deliver better care.
This blog explores how modernizing data estates can streamline patient risk stratification and enable hospitals to make more informed, timely decisions for improved patient outcomes.
Key Takeaways
- Patient risk stratification groups patients by risk levels to guide timely interventions and improve care delivery.
- Modernizing data estates consolidates clinical, operational, and social data, making risk assessments faster and more accurate.
- Integrated analytics, predictive models, and continuous monitoring enable proactive care for high-risk patients.
- Unified data systems streamline coordination, optimize resources, and support data-driven decision-making in hospitals.
- Upgraded data platforms prepare healthcare organizations for future challenges while improving patient outcomes and operational efficiency.
Before exploring how modern data platforms can transform healthcare delivery, it’s important to understand the foundation of patient risk stratification and why it matters for hospitals.
Introduction to Patient Risk Stratification and Its Importance
Patient risk stratification is the process of grouping patients based on their chances of developing health problems. It uses clinical data, demographic details, and patient history to separate patients into different risk levels.
The goal is to help care teams focus on patients who need more attention, plan treatment better, and provide the right care at the right time.
Studies show that most of patients account for nearly 50% of total healthcare costs, highlighting the need for accurate risk assessment to support timely decisions and avoid preventable hospital visits.
Here are the key benefits of effective patient risk stratification:
- Better Alignment with Clinical Programs: Patients are matched with the right care plans, such as preventive care or chronic disease management.
- Smarter Resource Use: Staff time, funds, and facilities are directed where they are needed most.
- Improved Patient Outcomes: Early action and targeted care reduce emergencies and support long-term health.
- More Coordinated Care: Different teams can work together with a shared view of patient risks, improving communication and treatment planning.
- Stronger Preventive Strategies: High-risk patients can be identified early for lifestyle programs or follow-ups, lowering future complications.
Example: Consider a hospital treating patients with diabetes and heart disease. With a proper risk stratification system, high-risk individuals can be identified early, placed in focused programs, and monitored closely, leading to better outcomes and more efficient hospital operations.
Also Read: Understanding the Benefits and Examples of Data Modernization Strategy
Once the importance of patient risk stratification is clear, the next step is to examine its core elements. These elements form the basis of effective risk assessments and guide care teams in making informed decisions.
Core Elements of Patient Risk Stratification in Hospitals

Risk stratification helps hospitals group patients based on their health needs, allowing teams to plan treatments, manage resources, and improve outcomes. By combining clinical data with patient inputs, hospitals can make better decisions for care delivery.
These elements include:
- Objective Data Analysis: Details like age, chronic illnesses (e.g., diabetes), lab results, and past admissions are collected to create a clear clinical profile for each patient.
- Subjective Data Inputs: Patient-reported health status, lifestyle habits, and self-assessments (e.g., pain levels or daily activity) give a fuller picture of individual health needs.
- Escalation and De-escalation Criteria: Defined rules adjust risk scores when conditions change, for example, worsening symptoms may move a patient to a higher-risk group for closer monitoring.
With these elements in place, hospitals can apply structured methods and modern tools to put risk stratification into action. The following approaches show how integrated platforms like Microsoft Fabric and Power BI can enhance precision and efficiency.
Methods for Effective Risk Stratification in Hospitals
Hospitals can improve patient outcomes by using modern data platforms for risk stratification. Tools like Microsoft Fabric, its Lakehouse, and Power BI can help connect data and provide clear insights for better patient care.
The following approaches help identify high-risk patients and guide timely interventions:
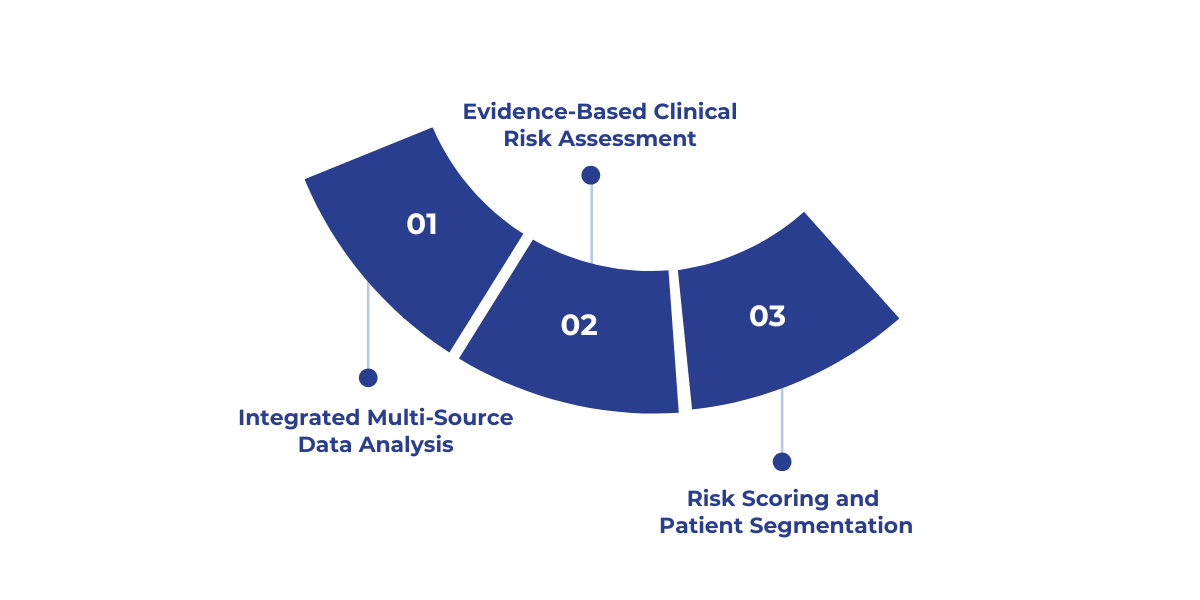
1. Integrated Multi-Source Data Analysis
Combine data from EHRs, lab results, imaging, wearable devices, and social determinants of health in a centralized Lakehouse. Integrating these sources provides a 360° view of each patient, improving risk assessment accuracy.
2. Evidence-Based Clinical Risk Assessment
Use validated clinical scoring systems, guidelines, and patient history to assess risk levels. Power BI dashboards make it easy to see risk levels and support data-driven decisions.
Combining structured clinical assessments with data from multiple sources ensures accurate identification of high-risk patients without relying solely on algorithms.
3. Risk Scoring and Patient Segmentation
Assign risk scores based on clinical, behavioral, and social information. With Power BI, hospitals can group patients into high, medium, and low-risk categories, helping prioritize care and resources effectively.
Using Microsoft Fabric and Power BI this way helps hospitals turn scattered data into clear insights, allowing faster interventions and better care for patients.
Looking to enhance patient risk stratification in your hospital? WaferWire helps modernize data estates to unify patient data, improve risk assessment, and enable timely, informed care decisions.
To support these methods at scale, hospitals need a strong technological foundation. Data estate modernization plays a crucial role by enabling better data integration, predictive analytics, and real-time insights.
How Can Data Modernization Improve Patient Risk Stratification?
Modern data platforms help hospitals enhance patient risk stratification by combining clinical, operational, and social data. This approach allows hospitals to identify high-risk patients, prioritize interventions, and improve overall outcomes.
To begin, hospitals need to consolidate and standardize data across all sources.
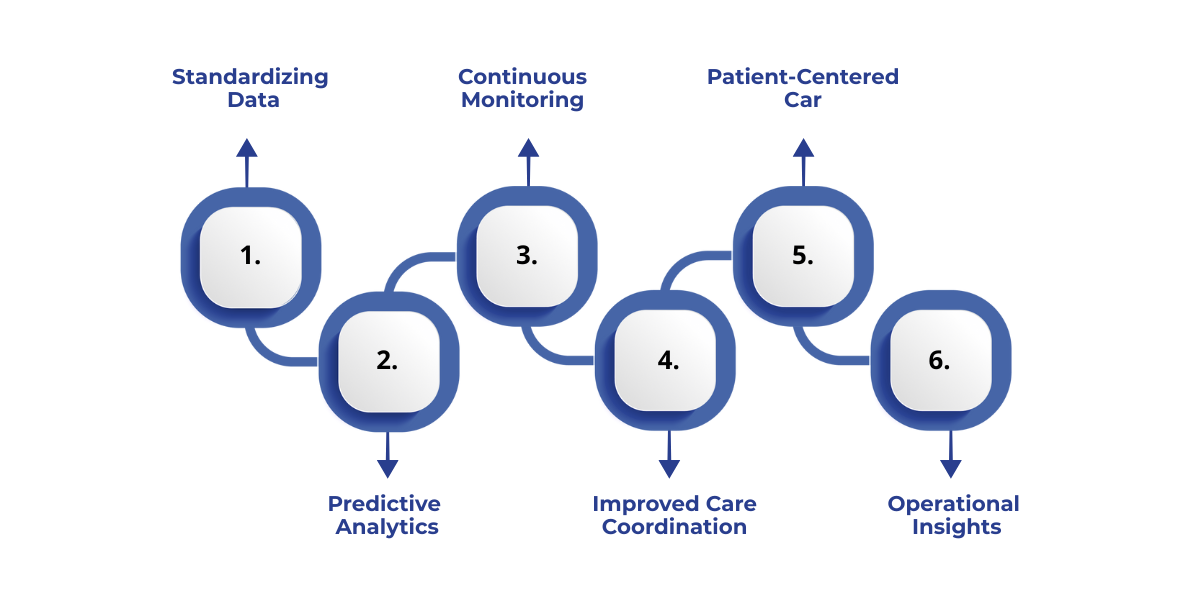
1. Consolidating and Standardizing Data
Hospitals can bring together data from EHRs, lab systems, imaging, and wearable devices to create a unified patient profile.
For example, a centralized platform can provide a comprehensive view of a patient’s medical history, lab results, and social determinants. With this clarity, hospitals can implement targeted programs for early intervention and preventive care.
Challenges:
- Integrating data from legacy infrastructures with differing formats can be complex.
- Data duplication and inconsistent coding may reduce accuracy.
Best Practices:
- Use ETL tools and modern AI integration frameworks to automate data harmonization.
- Implement data governance policies to maintain consistent standards and accuracy.
Once data is consolidated, predictive analytics becomes more effective.
2. Predictive Analytics for Risk Stratification
By analyzing integrated data, hospitals can forecast patient risks and flag those who need immediate attention.
Tools using AI and machine learning help generate accurate risk scores and personalized care plans, ensuring timely interventions for patients most likely to experience complications.
Challenges:
- AI models may produce biased results if the underlying data is incomplete or skewed.
- Clinicians may lack trust or understanding of predictive outputs.
Best Practices:
- Continuously validate and update models using diverse patient data.
- Include clinicians in model development and interpretation to build trust.
After identifying high-risk patients, hospitals benefit from continuous monitoring and feedback.
3. Continuous Monitoring and Feedback Loops
Modern platforms allow real-time tracking of patient vitals and outcomes through IoT devices, telehealth systems, and remote monitoring, such as Data analytics and AI tools. Hospitals can collect feedback, adjust care strategies quickly, and evaluate the effectiveness of interventions.
Challenges:
- Real-time monitoring generates massive data streams that can overwhelm IT systems.
- Ensuring patient privacy while collecting sensitive health data is critical.
Best Practices:
- Deploy scalable cloud-based platforms to manage high-volume data efficiently.
- Use encryption and strict access controls to protect patient information.
To strengthen these efforts, care coordination must be improved.
4. Improved Care Coordination
Integration of provider, payor, and community data supports smooth collaboration across teams.
For instance, modern workflows reduce duplication, streamline communications, and ensure that care plans are executed efficiently, enhancing patient outcomes and safety.
Challenges:
- Fragmented communication between departments may delay interventions.
- Resistance to workflow changes can hinder adoption.
Best Practices:
- Implement shared digital platforms for care teams to access and update patient records in real time.
- Provide training programs to ease transitions to new processes.
With better coordination, hospitals can expand proactive and patient-centered care.
5. Remote and Patient-Centered Care
Telehealth, virtual visits, and AI-driven engagement tools help hospitals reach high-risk or underserved populations. Analytics dashboards allow tracking trends, monitoring outcomes, and taking preemptive action to reduce complications.
Challenges:
- Limited patient access to digital tools can reduce reach.
- Maintaining quality of care remotely requires additional monitoring and support.
Best Practices:
- Offer patient education and technical support to increase digital engagement.
- Use hybrid care models combining in-person and remote interventions.
Finally, hospitals gain operational insights and decision support to optimize resource use.
6. Operational Insights and Decision Support
Hospitals can manage staffing, bed allocation, and patient flow more effectively. Data platforms provide actionable insights, enabling timely interventions and efficient use of hospital resources.
Challenges:
- Data overload may make it difficult to identify actionable insights.
- Poor alignment between operational data and clinical priorities can reduce impact.
Best Practices:
- Implement dashboards with customizable alerts for critical metrics.
- Regularly review performance indicators with clinical and operational teams to guide decision-making.
Also Read: Guide to Data Security and Privacy in Microsoft Fabric
Beyond risk scoring and analytics, modernizing the data estate drives widespread improvements across hospital operations. It strengthens decision-making, accelerates policy implementation, and enhances overall hospital performance.
How Data Estate Modernization Drives New Impacts in Hospitals?
Hospitals often face challenges in managing resources, coordinating teams, and making timely, data-driven decisions. Scattered information and complex workflows can slow operations and affect patient care.
Modernizing the data estate connects all information in one place, providing clear insights to optimize processes, allocate resources efficiently, and improve overall outcomes.
Here’s how it drives results:
Bringing it all together, modernizing data systems is not just about technology. it’s about enabling hospitals to identify high-risk patients early, allocate resources wisely, and deliver timely, high-quality care.
How WaferWire Supports Patient Risk Stratification with Modern Data Estates?
At WaferWire, we help hospitals enhance patient risk stratification by modernizing data estates for accurate, timely, and actionable insights. Here’s how we can assist:
- Unified Data Platform: Consolidate clinical, operational, and social data to create a single, comprehensive view of each patient for better risk assessment.
- Predictive Analytics: Use AI and machine learning models to identify high-risk patients early and generate personalized care plans.
- Real-Time Monitoring: Track patient vitals and outcomes with IoT and telehealth integrations, enabling proactive interventions.
- Risk Scoring & Segmentation: Categorize patients into high, medium, and low-risk groups for prioritized care and optimized resource allocation.
- Enhanced Care Coordination: Share real-time patient risk insights across care teams to streamline workflows and improve patient outcomes.
Additionally, our solution accelerators ensure a smooth transition to modern data-driven risk stratification:
- Data Consolidation & Governance: Standardize and harmonize data across multiple sources to maintain accuracy and consistency.
- Integration with Existing Systems: Seamlessly connect EHRs, lab systems, imaging, and wearable devices for a complete patient profile.
This approach helps hospitals identify high-risk patients faster, make data-driven decisions, and improve overall care efficiency.
Conclusion
By updating data systems and using technologies like AI, predictive analytics, and cloud platforms, hospitals can improve patient risk stratification. This helps identify high-risk patients early, use resources better, and provide faster, more accurate care.
Modern systems not only solve today’s challenges but also prepare hospitals for the future, improving patient outcomes and making care more efficient.
At WaferWire, we help hospitals upgrade their data systems and use smart tools to make risk stratification easier and more effective.
Contact us today to see how we can help improve care, reduce risks, and make your hospital ready for the future.
FAQs
1. What is patient risk stratification?
It’s the process of identifying patients based on their risk of complications or intensive care needs, helping hospitals prioritize care and improve outcomes.
2. How does data estate modernization improve patient risk stratification?
Modern data systems integrate and analyze diverse patient data, enabling more accurate risk scores and timely, proactive care.
3. What role does AI play in patient risk stratification?
AI predicts risks by analyzing large datasets, supporting early interventions, personalized care, and reduced hospital readmissions.
4. How can hospitals ensure accurate risk assessments?
By combining objective data (like age and chronic conditions) with subjective patient-reported information and continuously updating risk scores.
5. What impact does patient risk stratification have on healthcare outcomes?
It reduces emergency admissions, enhances patient engagement, improves chronic disease management, and lowers healthcare costs.
6. Can cloud-based solutions help with patient risk stratification?
Yes. Cloud platforms provide secure, real-time access to data, support analytics tools, and enable efficient, scalable risk stratification.
Subscribe to Our Newsletter
Get instant updates in your email without missing any news

Copyright © 2025 WaferWire Cloud Technologies




.png)